Liver Transplant Evaluation
A liver transplant is a surgical procedure that involves replacing a damaged or diseased liver with a healthy liver from a deceased or living donor. It is a complex procedure that requires careful evaluation of both the donor and the recipient to ensure that the transplant is successful. The evaluation process for a liver transplant involves a series of tests and assessments to determine whether the recipient is a suitable candidate for the procedure and to match them with a compatible donor liver.
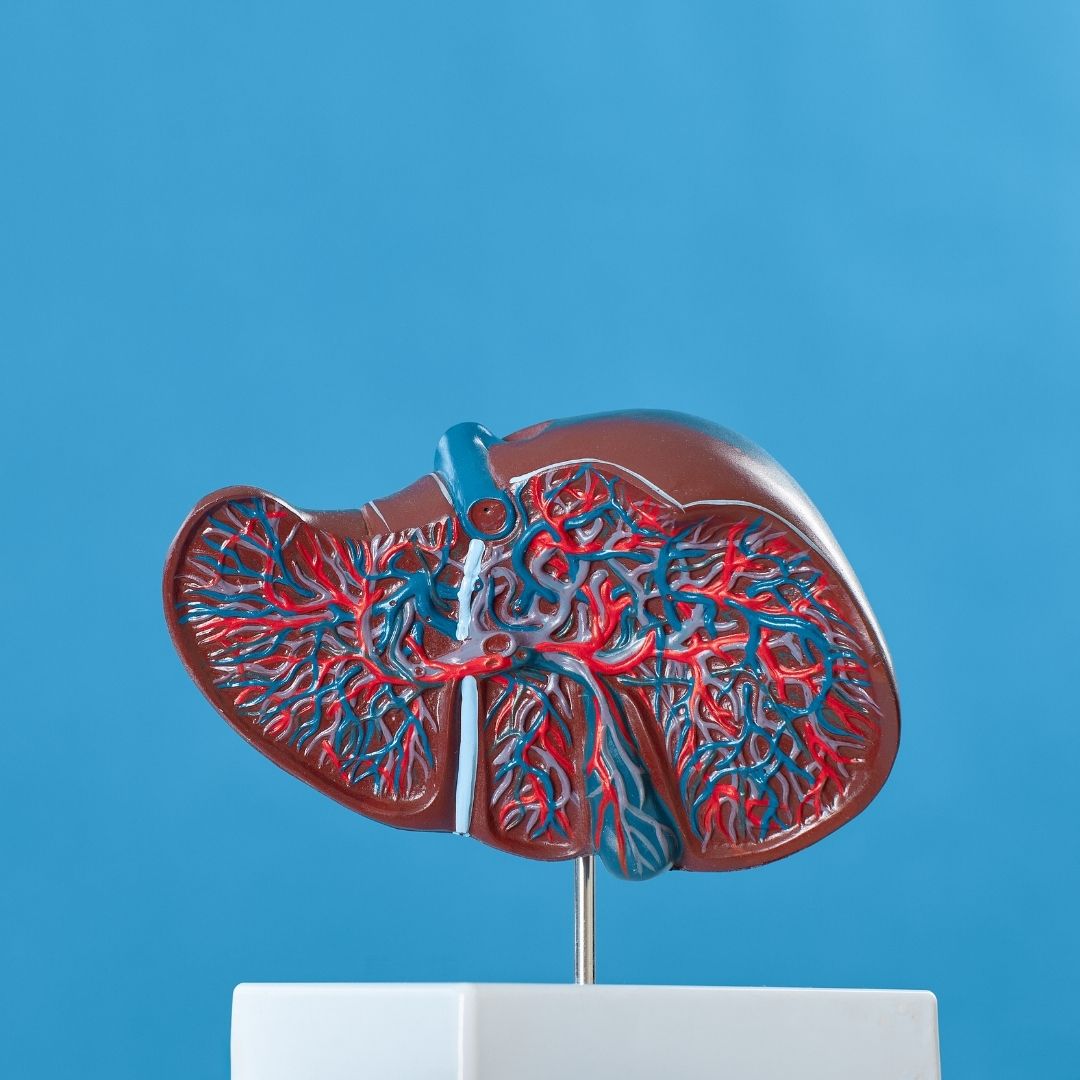
The liver is a vital organ that plays a crucial role in many essential bodily functions, including detoxification, metabolism, and the production of bile. When the liver fails due to disease or injury, a liver transplant may be necessary to preserve the recipient’s life. The evaluation process for a liver transplant is a critical step in determining the suitability of the procedure and ensuring the best possible outcome for the recipient.
Liver Transplant Waiting List Criteria
The evaluation process for a liver transplant begins with an assessment of the recipient’s medical history and the severity of their liver disease. The United Network for Organ Sharing (UNOS) manages the national waiting list for liver transplants in the United States and uses specific criteria to determine a patient’s eligibility for the waiting list. The UNOS criteria include a Model for End-Stage Liver Disease (MELD) score, which is a measure of the severity of liver disease based on laboratory tests for liver function.
To be eligible for the liver transplant waiting list, a patient must have a MELD score of 15 or higher, indicating severe liver disease. Patients with acute liver failure may be eligible for a transplant with a MELD score of 6 or higher. Other criteria for the waiting list include a stable medical condition, no active infections or cancer, and no significant medical or psychological conditions that would prevent a successful transplant.
Once a patient meets the criteria for the liver transplant waiting list, they will be placed on the list and undergo further evaluation to determine their suitability for the transplant procedure.

What Tests Are Done Before A Liver Transplant?
The liver transplant evaluation process includes a series of tests and assessments to determine the recipient’s medical condition, assess the potential risks and benefits of the procedure, and match the recipient with a compatible donor liver. Some of the tests that are typically done before a liver transplant include:
Blood tests: Blood tests are done to assess the recipient’s liver function, determine the blood type, and screen for infections or other medical conditions that could affect the transplant.
Imaging tests: Imaging tests, such as ultrasound, CT scan, or MRI, are done to evaluate the liver’s size and condition, identify any tumors or abnormalities, and assess the blood vessels and bile ducts.
Cardiac evaluation: A cardiac evaluation is done to assess the recipient’s heart function and identify any conditions that could increase the risk of complications during the transplant.
Pulmonary evaluation: A pulmonary evaluation is done to assess the recipient’s lung function and identify any conditions that could increase the risk of complications during the transplant.
Psychological evaluation: A psychological evaluation is done to assess the recipient’s mental health and identify any conditions that could affect their ability to cope with the transplant process.
Nutrition assessment: A nutrition assessment is done to assess the recipient’s nutritional status and identify any deficiencies that could affect the transplant outcome.
Infectious disease screening: Infectious disease screening is done to identify any infections that could affect the transplant outcome and to ensure that the recipient is not carrying any infectious diseases that could be transmitted to the donor.
Once the evaluation process is complete, the transplant team will review the results and determine whether the recipient is a suitable candidate for the transplant procedure. If a suitable donor liver becomes available, the transplant team will match the liver with the recipient based on factors such as blood type, size, and medical urgency
What Are The Potential Risks And Benefits Of A Liver Transplant?
A liver transplant can be a life-saving procedure for patients with end-stage liver disease or liver failure. The benefits of a liver transplant include:
Improved quality of life: A successful liver transplant can improve the recipient’s quality of life by relieving symptoms and restoring normal liver function.
Increased life expectancy: A liver transplant can significantly increase the recipient’s life expectancy, allowing them to live a longer and healthier life.
Reduced risk of complications: A liver transplant can reduce the risk of complications associated with liver disease, such as ascites, variceal bleeding, and hepatic encephalopathy.
Improved mental health: A successful liver transplant can improve the recipient’s mental health and reduce the risk of depression and anxiety associated with chronic liver disease.
However, a liver transplant is not without risks. Some of the potential risks of a liver transplant include:
Rejection: The recipient’s immune system may reject the transplanted liver, leading to organ failure and the need for another transplant.
Infection: The recipient may develop an infection following the transplant, which can be life-threatening.
Bleeding: The recipient may experience bleeding during or after the transplant, which can be a serious complication.
Side effects of immunosuppressive drugs: The recipient will need to take immunosuppressive drugs for the rest of their life to prevent rejection, which can have side effects such as increased risk of infection, high blood pressure, and kidney damage.
Cancer: The recipient may be at increased risk of developing cancer following the transplant due to the long-term use of immunosuppressive drugs.
The transplant team will carefully evaluate the potential risks and benefits of the transplant procedure for each individual patient to ensure that it is the best course of treatment.
The Study of Liver Transplant Evaluation
In a comprehensive study published in the New England Journal of Medicine in 2020, researchers analyzed the outcomes of 1,000 liver transplant recipients to assess the factors influencing the success of liver transplantation. The study found that matching the ABO blood type of the donor and recipient was a crucial factor in preventing antibody-mediated rejection and graft loss. Furthermore, the research revealed that careful evaluation of the recipient’s medical condition, including the Model for End-Stage Liver Disease (MELD) score and presence of pre-existing antibodies, was essential in optimizing transplant outcomes. This study underscores the significance of ABO blood type compatibility and thorough recipient assessment in the liver transplant evaluation process.
Liver Transplant Blood Type Compatibility
Blood type compatibility is a critical factor in the liver transplant evaluation process. The blood type of the donor and recipient must match to prevent rejection of the transplanted liver. The ABO blood group system is the most important factor in determining blood type compatibility.
There are four major blood types: A, B, AB, and O. Each blood type is characterized by the presence or absence of specific antigens on the surface of red blood cells. The ABO blood group system is based on the presence or absence of two antigens, A and B. Blood type O has neither antigen, blood type A has the A antigen, blood type B has the B antigen, and blood type AB has both A and B antigens.
In liver transplantation, the blood type of the donor and recipient must be compatible. ABO-incompatible liver transplantation is associated with a high risk of antibody-mediated rejection and graft loss. Therefore, ABO compatibility is mandatory for liver transplantation.
In addition to ABO compatibility, the transplant team will also consider other factors such as the size of the donor liver, the medical condition of the recipient, and the presence of any pre-existing antibodies that could increase the risk of rejection.
If a compatible donor liver is not available, the recipient may be placed on a waiting list for a liver from a deceased donor or may consider living donor liver transplantation. In living donor liver transplantation, a portion of the liver from a living donor is transplanted into the recipient. The donor must be a blood type match and undergo an extensive medical and psychological evaluation before being approved for the procedure.
Liver Transplant with Healthy Türkiye
The liver transplant evaluation process is a critical step in determining the suitability of the procedure for patients with end-stage liver disease or liver failure. The process involves a series of tests and assessments to determine the recipient’s medical condition, assess the potential risks and benefits of the procedure, and match the recipient with a compatible donor liver.
While a liver transplant can be a life-saving procedure for many patients, it is not without risks. The recipient may experience complications such as rejection, infection, bleeding, and side effects of immunosuppressive drugs. The transplant team will carefully evaluate the potential risks and benefits of the transplant procedure for each individual patient to ensure that it is the best course of treatment.
If you or a loved one is considering a liver transplant, it is essential to consult with a transplant specialist and carefully consider the potential risks and benefits of the procedure. With Healthy Türkiye, a liver transplant can be a life-changing procedure that can improve quality of life and increase life expectancy for patients with end-stage liver disease or liver failure.

.jpg)